The landscape of COVID-19 vaccination recommendations in the United States is experiencing notable shifts, especially concerning the pediatric population. Recently, a cohort of U.S. pediatricians has proposed guidance that diverges from the prevailing advice issued by the Centers for Disease Control and Prevention (CDC). This divergence sparks critical conversations about vaccine policy, safety, efficacy, and the best interests of children across the nation. To understand the full scope of this departure, it’s essential to analyze the motivations behind the pediatricians’ recommendations, compare them with CDC guidelines, and explore the implications for parents, healthcare providers, and policymakers alike.
Background: The Evolution of COVID-19 Vaccination Policies
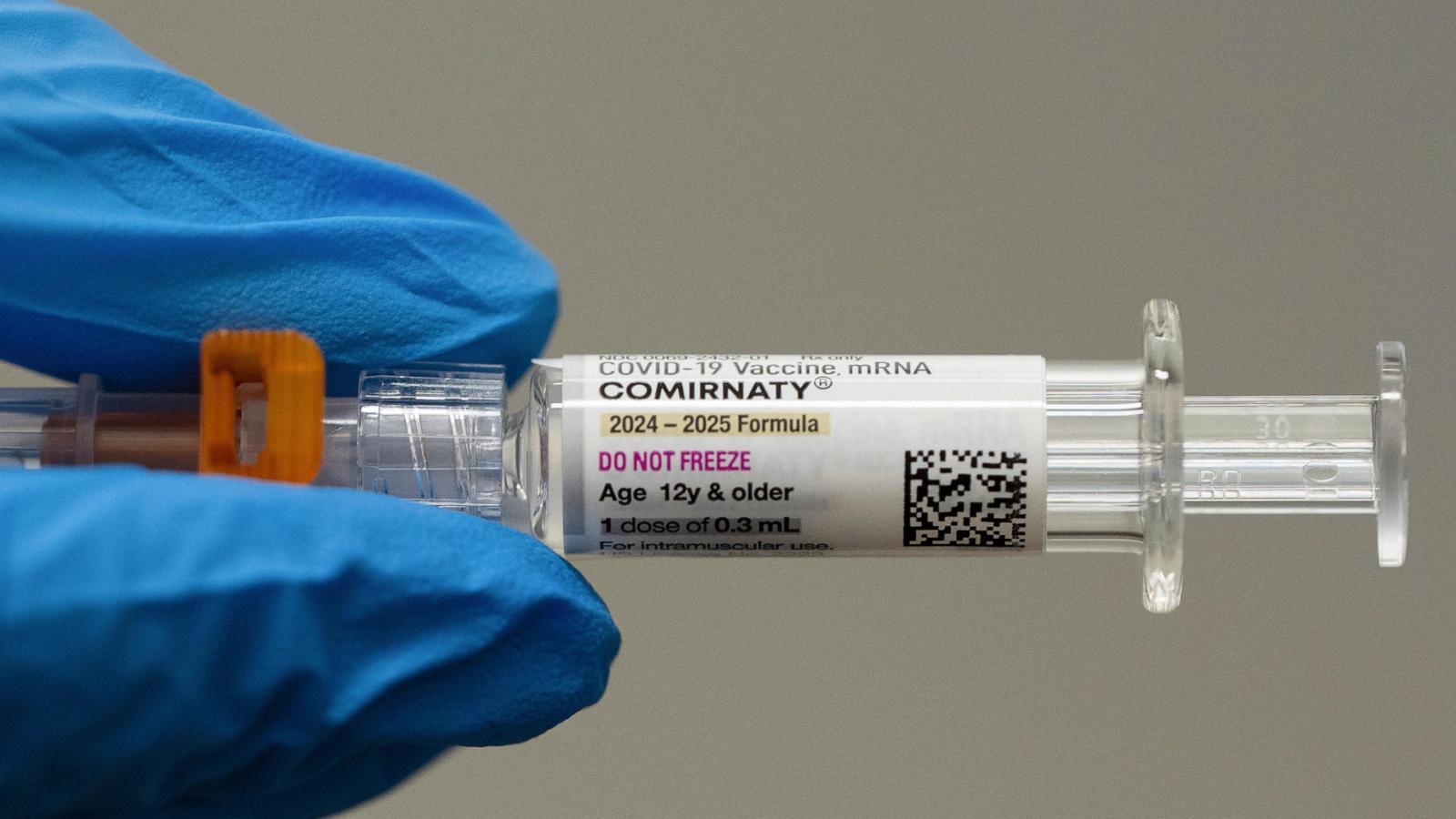
Since the onset of the COVID-19 pandemic, vaccination strategies have evolved rapidly. Initially focused on high-risk adults, the U.S. pivoted to include children as vaccine safety and efficacy data became available. The CDC has traditionally been the authoritative body providing nationwide guidelines, emphasizing widespread immunization to curb transmission and protect vulnerable populations. Their advice has been rooted in extensive clinical trials, epidemiological data, and expert consensus.
However, as the pandemic persisted, new data, emerging vaccine formulations, and real-world experiences prompted ongoing re-evaluation of recommendations. This dynamic environment has opened the door for diverse clinical opinions and, consequently, policy debates.
The Divergence: Pediatricians’ New Recommendations
In recent months, a notable subset of U.S. pediatricians has begun advocating for a more cautious or modified approach to COVID-19 vaccination for children. According to reports from ), these pediatricians are emphasizing caution over immediate widespread vaccination, especially among certain age groups. Their stance is often driven by concerns about vaccine safety, potential side effects, and the long-term effects which, despite extensive clinical trials, remain somewhat unknown for children.
The new guidance calls for **more individualized risk assessments** and suggests that parents and healthcare providers carefully consider the child’s health status before vaccinating. Some pediatricians recommend delaying or spacing out booster doses or even question the routine need for vaccination in certain low-risk groups.
Key Differences Between Pediatricians’ Recommendations and CDC Guidelines
- Safety Concerns: While the CDC maintains that COVID-19 vaccines are safe and effective for children aged 5 and above, some pediatricians express reservations regarding rare adverse events like myocarditis, especially in younger boys. They advocate for more comprehensive long-term studies before universal recommendations.
- Vaccine Frequency and Dosage: The CDC recommends the standard dosing schedule, including booster shots, for eligible children. In contrast, some pediatricians prefer a more conservative approach—advocating for fewer doses or extended intervals to monitor potential side effects.
- Risk-Based Approach: CDC guidelines promote vaccination broadly, regardless of individual risk factors. Conversely, pediatricians with divergent views suggest tailoring vaccination based on individual health status, family exposure risks, and community transmission levels.
- Public Messaging: The CDC emphasizes vaccination as a tool for community-level immunity, while dissenting pediatricians caution against overgeneralization and stress informed decision-making.
Reasons Behind the Divergence
Understanding why some pediatricians are recommending deviations from CDC guidance requires examining several factors:
1. Safety and Long-term Data Gaps
Despite the extensive testing protocols that vaccines underwent, concerns persist about rare side effects and long-term consequences in children. Pediatricians advocating for cautious use argue that more data are might needed before endorsing universal vaccination.
2. Evolving Viral Dynamics
The emergence of new variants, such as Omicron, has altered the risk landscape. Pediatricians question whether the benefits of vaccination outweigh the risks, especially among healthy children who are less likely to suffer severe disease.
3. Natural Immunity Considerations
Some experts highlight the role of natural immunity from prior infection, suggesting that for some children, vaccination might be less necessary, especially if they have already recovered from COVID-19.
4. Parental Autonomy and Informed Consent
Advocates for more conservative vaccination advice emphasize the importance of respecting parental choice and providing comprehensive information, rather than broad mandates.
Implications for Policy and Public Health
This divergence in recommendations raises complex questions about public health management:
**Balancing Risks and Benefits:** Policymakers and health authorities must reconcile the need for widespread vaccination with concerns about safety and individual choice. Clear, transparent communication is key to maintaining public trust.
**Uniformity vs. Flexibility:** Strict adherence to CDC guidelines might overlook individual risks and circumstances, while more flexible, evidence-informed pediatric recommendations could help in addressing specific concerns.
**Vaccine Hesitancy:** Mixed messages from various medical leaders can fuel hesitancy among parents, potentially undermining vaccination campaigns. Ensuring consistent messaging grounded in the latest evidence is crucial.
**Monitoring and Research:** Ongoing surveillance and research are vital to assess vaccine safety, especially for children, and to inform future updates to recommendations.
The Path Forward: Navigating Different Perspectives
In light of these differing opinions, several strategies can help harmonize efforts:
– Enhanced Communication: Health authorities should actively engage with pediatricians and communities to explain the evidence base and address concerns.
– Personalized Medical Guidance: Emphasize individualized assessment, allowing healthcare providers to adapt recommendations based on each child’s health status.
– Continued Data Collection: Invest in research to fill data gaps, particularly on long-term safety and efficacy in children.
– Parental Involvement: Support informed decision-making through transparent, accessible information tailored to families’ needs.
Conclusion
The recent divergence between U.S. pediatricians’ COVID-19 vaccine recommendations and CDC guidance underscores the complexity of pandemic management in pediatric populations. It reflects ongoing debates about vaccine safety, efficacy, risk stratification, and individual rights. As science continues to evolve, it remains critical that health guidance is adaptable, evidence-based, and transparent—balancing public health goals with respect for individual and parental choices. Fostering open dialogue among health professionals, policymakers, and families will ultimately help navigate this nuanced landscape.
For more updated news please keep visiting Prime News World.








